Faculty takes on Alzheimer’s
Biomedical engineers use new imaging technology to better understand disease
By Meghan King
text block 1
In 2020, the U.S. Centers for Disease Control estimated 5.8 million Americans aged 65 years or older had Alzheimer’s disease (AD). The agency expects this number to almost triple to 14 million people by 2060.
Despite the huge number of people impacted by the disease, scientists are still not sure what exactly causes Alzheimer’s. Researchers strive to get better ideas about the underlying mechanism(s) of the disease and explain why some people’s brains become unreliable and make them forget things and even loved ones.
Multiple researchers within the Richard and Loan Hill Department of Biomedical Engineering are trying to improve our understanding of AD, diagnostics, and treatments to slow down disease progression, and identify the causes of AD and other age-related deterioration.
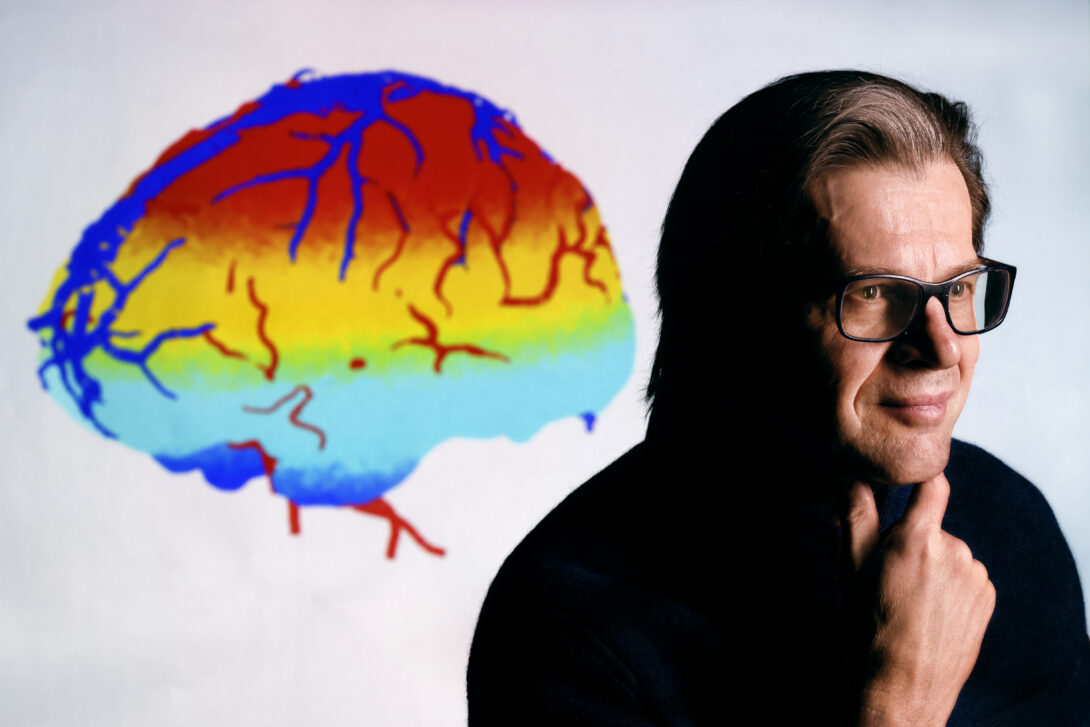
“Alzheimer’s disease is a big health burden,” said Professor Andreas Linninger. “It’s a burden in the sense of the monetary cost, but it also not only changes the life of the patient, but it changes the life of the whole family.”
Impact of blood flow and oxygen
Linninger recently received a grant from the National Institutes of Health’s National Institute of Aging (NIA) to use advanced imaging techniques to detect whether there are subtle changes in blood flow and if oxygen extraction is altered in brains that are at risk of disease or that have suffered complications.
This grant, he said, has been three years in the making as they were told that despite high scores when it was first presented to the NIA, there were doubts about the possibility of creating a digital model of both the mouse and human brains.
“We wanted to create these digital models to understand fundamentally what the changes in hemodynamics and oxygen extraction are that the old brain experiences and could these changes be used to explain the cognitive decline we see in some people,” Linninger said.
Some of those doubts included that capturing the complexity of the capillary network in a human or in a mouse brain would be impossible and that the computational models would create too many equations to solve.
However, during their preparatory work, they created a silico digital mouse brain model to chart all blood vessels in the mouse and then computed blood flow and pressure. They were finally given the $3.5 million grant in December 2022 by the NIA.
Linninger explained that through Fred Lesage of Polytechnique Montreal’s work on oxygenation in aging populations, they may not only be able to show how the process works in the brain but also how it is related to brain diseases.
“That is maybe the unusual thing,” Linninger said, “We were not engineers who decided we needed to make a contribution in aging brain research, we were engineers who wanted to understand the fluid mechanics of the brain, but that happens to also be a potential reason why the brain fails.”
This project is being conducted with Lesage of Polytechnique Montréal in Canada and Bill Rooney of the Oregon Alzheimer’s Disease Center at Oregon Health and Science University.
Some of the patient benefits of Linninger’s research could be improved and earlier diagnostics, which would allow patients to start treatments as soon as possible.
“There are other pharmacological avenues that can be pursued as soon as you understand the fundamental principle of what goes wrong,” Linninger said.
text block 2
Palpating the brain
Associate Professor Dieter Klatt has been looking into changes occurring inside the brains of AD model mice using magnetic resonance elastography (MRE), which is an image-based method like palpation, a common practice for physicians.
Klatt explained palpation is “one of the oldest diagnostic methods that doctors have used for centuries around the world that when you report a problem, they use their hands to feel if the tissue is soft,” Klatt said. “Usually, healthy tissue is soft. Palpation was always done by manual probation with the fingers, but MRE can create images that visualize the stiffness, so when you see the different tones in the image they indicate if it’s soft or hard.”
Klatt added he and his team are still working to figure out what diseases are sensitive to this technique.
A recent study from his team used two groups of live mice, including a control group of healthy mice and a group of genetically altered mice with AD. During the study, they used MRE to determine the mechanical properties in the mouse brain and the reduction of the stiffness in the brain.
“Using our technique, we could show that there is a difference in the stiffness of the brain of an Alzheimer’s disease mouse, compared with a healthy mouse,” Klatt said.
He added in the future MRE could provide a way to non-invasively detect and monitor AD in humans.
quote from linninger
Alzheimer’s disease is a big health burden … It not only changes the life of the patient, but it changes the life of the whole family.
| Professor of biomedical engineering
text block 3
A new view
Richard & Loan Hill Professor Xincheng Yao is supported by multiple NIH National Eye Institute grants for functional imaging of the retina. As one part of the central nerve system, the retina offers a unique window to enable noninvasive assessment of neurodegeneration due to AD.
Yao is collaborating with Professor James Lee on a grant proposal to combine the imaging assessment of AD using optical coherence tomography angiography (OCTA). They are also attempting to identify if photo-biomodulation can be used to prevent or delay the neurodegeneration in the retina correlated with the disease.
Yao works with optical coherence topography (OCT) and OCTA, which image the microvasculature of the retina and the choroid. OCTA images show the difference in functional blood flow over time, and they can enhance the visibility of blood vessels.
“We use the blood flow information to enhance the visibility of individual blood vessels so you can compare OCTA to OCT,” Yao said.
Lee and Yao are using functional OCTA to check the retinal degenerations in an AD mouse model. They can use optical imaging technology to access the eye without damaging it or the brain. Using the quantitative analysis of the blood vessels, like density or diameter, will show that some optical features may reflect the retinal defects or are correlated with that function in the future.
Yao said that he and Lee are hoping for earlier detection of Alzheimer’s Disease and examine the progression of the disease or the treatment outcome over time without damage to the animal or human body.
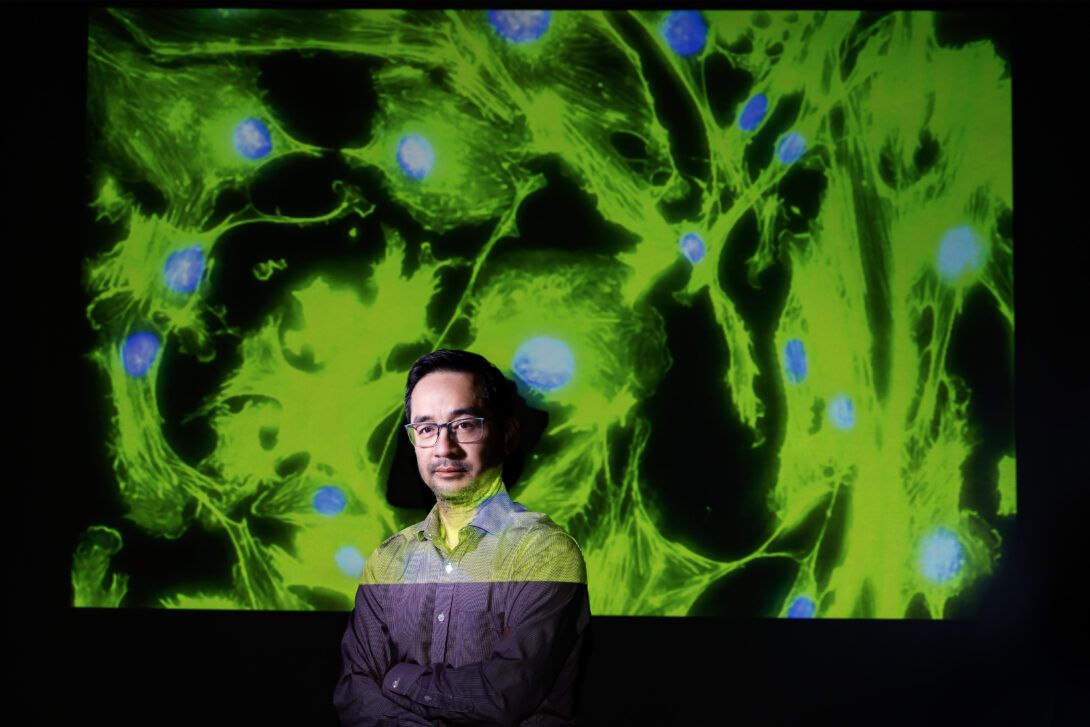
Examining the brain’s defenses
Over the past 15 years, Lee has received NIH grants to support his Alzheimer’s research. As a traditionally trained engineer, Lee applies engineering techniques and principles to investigate the roles of membrane biophysics and mechanics in the pathology of AD.
Through the support of his current NIH grant, Lee is looking into the blood-brain barrier, a controlled border made of endothelial cells that allow transports of biological materials selectively going in and out of the brain, which are essential for the brain’s metabolic activity and neuronal function.
He is using cell models to see what happens if we allow endothelial cells that have direct interactions with toxic proteins found in Alzheimer’s brains—amyloid beta peptide and tau.
When using endothelial cells to make a blood-brain barrier model, these toxic proteins make the model become leaky and stickier to white cells. This model helps explain why increased white blood cells from peripheral blood to get to the brain tissue of AD patients, which may further exacerbate the disease.
“When too many white blood cells exist in the brain, they might cause high levels of neuroinflammatory and oxidative stress,” Lee said.
The blood-brain barrier plays a key role in the generation and maintenance of chronic inflammation during AD.
Inflammation, Lee said, plays a key role in many neurodegenerative diseases, such as Alzheimer’s. It is a double-edged sword as too much inflammation is not good and will exacerbate the disease, however, too low inflammation might prevent healing.
Throughout all his research, Lee is looking to slow down the progression of Alzheimer’s Disease in patients.